There’s a revolution happening in psychiatry, and it’s rewriting everything we thought we knew about mental health. At the centre of it is a deceptively simple idea: what if depression, anxiety, and other mental illnesses aren’t just chemical imbalances in your brain, but energy problems?
Dr. Christopher Palmer, a Harvard psychiatrist, is leading this movement with his book Brain Energy, and the implications are profound.
The Power Plant Problem
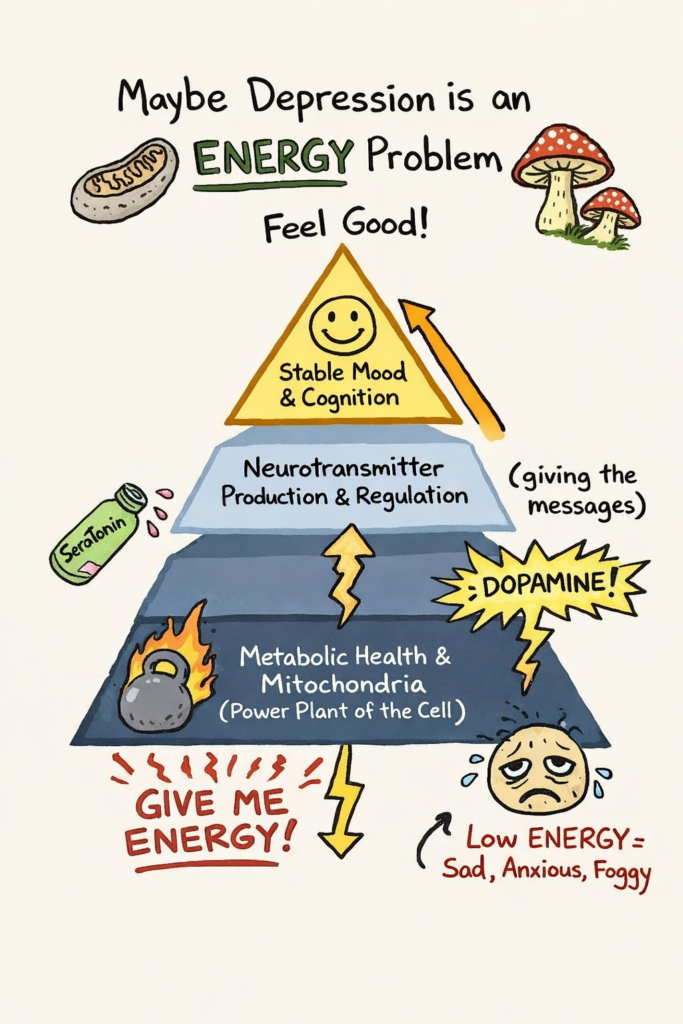
For decades, psychiatry has been obsessed with the synapse, which is the tiny gap between neurons where neurotransmitters like serotonin and dopamine do their work. The story was that too little serotonin equals depression. So fix the serotonin, fix the problem. It’s clean, it’s simple, and for many people, SSRIs (antidepressants that increases serotonic) do offer some help.
But for the roughly 30-40% of patients who don’t respond to traditional treatments, this model falls apart. Palmer and a growing number of researchers in the emerging field of Metabolic Psychiatry are asking a more fundamental question: What powers the synapse in the first place?
The answer is mitochondria – those tiny organelles you learned about in high school biology. They’re often called the “powerhouses of the cell”, but we are now realising that they are much more than this. They are more like the “CEO of the cell”, not only transforming and producing energy, but also orchestrating how that energy is used. When mitochondrial function breaks down, whether from genetics, inflammation, insulin resistance, or chronic stress, the brain literally runs out of energy. Neurotransmitters might be the messengers, but without fuel, the messages can’t get sent.
This isn’t just theoretical. When your brain’s energy metabolism falters, you get the symptoms we call mental illness: brain fog, emotional instability, depression, and in severe cases, psychosis. Mental health and physical health aren’t separate systems. They’re two sides of the same metabolic coin.
Revolutionary
Palmer’s framework unifies mental and physical health under one roof. This is why exercise helps both depression and diabetes. Why meditation improves anxiety and reduces inflammation. Why sleep deprivation wrecks both your mood and your blood sugar. They’re all connected through metabolism.
The practical implications are immediate. Instead of just targeting neurotransmitters, we can address the underlying energy disfunction through diet (particularly ketogenic and intermittent fasting approaches), exercise, sleep optimisation, and stress management. Palmer shares case studies of patients whose psychiatric conditions dramatically improved through metabolic interventions, even people who’d exhausted conventional options.
From Theory to Data
Recent pilot studies are starting to back this up with hard numbers. A 2024 Stanford trial tested a ketogenic diet in adults with schizophrenia or bipolar disorder who also had metabolic issues. Among those who stuck with it, metabolic syndrome resolved completely, and psychiatric symptoms improved by about 31%. In young adults with major depression, a ketogenic intervention led to 60-70% reductions in depression scores within weeks.
The mechanism appears to involve ketones – specifically beta-hydroxybutyrate (BHB) – doing more than just providing alternative brain fuel. BHB acts as a signalling molecule that shifts gene expression, increasing GABA (your brain’s calming neurotransmitter) and decreasing glutamate (the excitatory one). Brain imaging studies have shown roughly 10-12% decreases in excitatory glutamate in emotional regulation centres during ketogenic interventions.
Enter the Mushrooms
As someone who’s obsessed with fungi, this new metabolic framework of mental health has helped me understand the positive health effects of mushrooms – both functional and ‘magic’ ones. Recent research (which I’ve written about previously) is revealing metabolic effects of psilocybin that align perfectly with Palmer’s framework. Studies show psilocybin extends cell life, promotes metabolic health in animal models, and even biohacker Bryan Johnson has reported positive metabolic effects from his personal experiments.
This suggests that both functional mushrooms (like lion’s mane and cordyceps, known for their mitochondrial support and neuroprotective properties) and psilocybin mushrooms may be working on mental health through metabolic pathways. Not just through direct effects on serotonin receptors, but by improving how brain cells generate and use energy.
It’s a first-principles approach: instead of asking “which neurotransmitter is off?”, we’re asking “is the cellular machinery working?”
The Bigger Picture
We’re in the midst of a global mental health crisis. Mental illnesses are rising globally, and our current treatments, while helpful for some, leave millions without adequate relief. Palmer’s metabolic psychiatry offers a new paradigm: treat the energy system, and you may resolve the mental health symptoms.
This doesn’t mean throwing out psychiatric medications or therapy. It means adding a crucial physiological layer to existing models. It’s seeing the patient as a whole system rather than focusing on individual parts or chemicals.
For patients who’ve exhausted standard options, this reframing offers genuine hope. It also validates what many people intuitively know: that taking care of your body – through nutrition, movement, sleep, stress reduction, and potentially mushrooms – isn’t separate from taking care of your mind. It’s all one interconnected system, powered by the same metabolic processes.
The revolution is metabolic. It’s just beginning. And mushrooms could play a big role.
Note: Metabolic psychiatry is still an emerging field. Ketogenic interventions and psilocybin treatments remain experimental for most psychiatric conditions and should only be pursued under expert medical supervision, with appropriate monitoring.